Understanding Deep Vein Thrombosis (DVT)
Deep vein thrombosis, commonly known as DVT, is a medical condition characterized by the formation of a blood clot in a deep vein, usually in the legs. This condition can lead to significant complications if not addressed promptly, including the risk of pulmonary embolism when the clot dislodges and travels to the lungs.
DVT often develops due to prolonged periods of inactivity, such as long flights or extended bed rest after surgery or illness. However, other factors like obesity, certain medications, and genetic predispositions can also play a role.
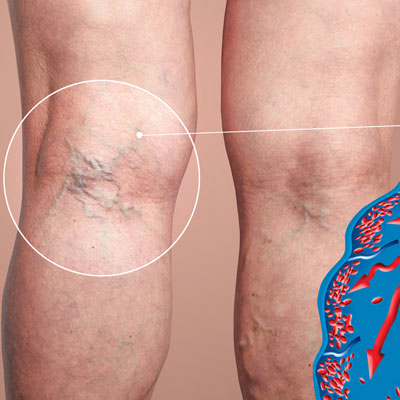
Symptoms may include swelling, pain, and redness in the affected area; however, some individuals may be asymptomatic. Early diagnosis is crucial for effective treatment and prevention of serious outcomes.
Understanding the risk factors and recognizing symptoms can empower individuals to seek timely medical attention. Awareness of DVT is essential for those at higher risk and plays a vital role in public health strategies aimed at reducing its incidence.
Common Symptoms of DVT
Swelling – Often in one leg, the affected area may appear swollen and feel tense or tight.
Pain or Tenderness – Affected individuals may experience pain or tenderness in the leg, which often starts in the calf and can feel like cramping or soreness.
Red or Discolored Skin – The skin over the affected area might appear red, bluish, or discolored compared to the surrounding skin.
Warmth – The skin around the thrombosis site may feel warmer than other areas of the leg.
These symptoms can vary from person to person, and it’s important to seek medical attention if DVT is suspected.
Risk Factors and Causes of DVT
Deep vein thrombosis (DVT) is a condition characterized by the formation of a blood clot in a deep vein, typically in the legs. Several risk factors significantly increase the likelihood of developing DVT.
Prolonged periods of inactivity pose a major risk. This includes long flights, extended bed rest after surgery, or a sedentary lifestyle. When blood circulation slows down due to immobility, it can lead to clot formation.
Age also plays a crucial role; individuals over 60 are at higher risk. Additionally, certain medical conditions such as cancer and heart disease can predispose patients to DVT by affecting blood flow and coagulation.
Hormonal factors are important as well; for instance, women taking oral contraceptives or hormone replacement therapy may experience an increased risk. Obesity is another contributing factor that places added pressure on veins in the legs.
Family history of DVT can indicate genetic predispositions to clotting disorders. Together, these elements highlight the importance of being aware of personal health and lifestyle choices to mitigate the risks associated with this potentially serious condition.
Diagnosis Methods for DVT
Diagnosis of Deep Vein Thrombosis (DVT) involves several methods to ensure accurate identification of the condition. One common approach is a thorough medical history and physical examination. Physicians often look for symptoms such as swelling, pain, and warmth in the affected limb.
Ultrasound imaging is the most frequently used method for diagnosing DVT. This non-invasive technique uses sound waves to create images of blood flow in the veins, helping to identify any clot presence.
In certain cases, doctors may recommend a D-dimer test. This blood test measures levels of a substance that’s released when a blood clot breaks down. Elevated levels can indicate potential clotting issues though further tests are usually needed for confirmation.
Other diagnostic tools include venography, where a contrast dye is injected into a vein to make it visible on X-rays, and MRI scans that provide detailed images without radiation exposure.
Each method has its advantages and limitations, making it crucial for healthcare providers to use a combination of techniques based on individual patient circumstances. Early detection plays a vital role in effective treatment and prevention of complications associated with DVT.
Treatment Options for DVT
Deep vein thrombosis (DVT) requires timely and effective treatment to prevent complications, such as pulmonary embolism. The primary approach typically involves anticoagulant medications, commonly referred to as blood thinners. These medications help prevent the clot from growing larger and reduce the risk of new clots forming.
In some cases, healthcare providers may recommend thrombolytics, which are more aggressive treatments aimed at dissolving the clot quickly. This option is usually reserved for severe cases or when there is an immediate threat to health.
For patients with significant symptoms or those who cannot take anticoagulants, a temporary inferior vena cava (IVC) filter may be inserted. This device prevents clots from traveling to the lungs while allowing blood flow through the veins.
Compression stockings are also an essential component of DVT management. They promote circulation in the legs and can help prevent swelling and discomfort.
Lifestyle changes like increased mobility, hydration, and regular exercise can further support recovery and enhance overall vascular health. Close monitoring by healthcare professionals is crucial throughout treatment to ensure optimal outcomes and minimize risks associated with DVT.
Preventive Measures Against DVT
Deep vein thrombosis (DVT) is a serious condition where blood clots form in the deep veins, often in the legs. Fortunately, there are several effective preventive measures that can help reduce the risk of developing DVT.
Firstly, physical activity plays a key role. Regularly engaging in exercise, such as walking or stretching, helps promote healthy blood circulation. For individuals who must remain sedentary for long periods, such as during long flights or car rides, it’s essential to make periodic stops or take breaks to move around.
Hydration is another critical factor. Drinking plenty of water keeps the blood from becoming too thick and reduces clot formation risks. Additionally, avoiding alcohol and caffeine can also be beneficial, as both can lead to dehydration.
Wearing compression stockings is highly recommended for those at higher risk or those traveling long distances. These stockings provide gentle pressure to help improve blood flow in the legs.
Lastly, it’s necessary for individuals with pre-existing health conditions or a history of DVT to consult with their healthcare providers about appropriate medications or preventative therapies. By taking these proactive steps, one can significantly lower their chances of experiencing DVT.
Conclusion
In summary, Deep Vein Thrombosis (DVT) is a serious medical condition that can lead to severe complications if left untreated. Recognizing the symptoms, understanding the risk factors, and seeking prompt treatment are crucial steps in managing this condition effectively. Various treatment options are available, ranging from anticoagulants to lifestyle modifications, which can significantly reduce the risks associated with DVT. It is essential for individuals at higher risk to engage in preventive measures and stay informed about their health. By prioritizing awareness and proactive healthcare, we can combat the dangers of DVT together—don’t hesitate to consult a healthcare professional if you suspect you may be at risk.
FAQs
Is DVT life-threatening?
Yes, DVT can be life-threatening if the clot breaks loose and travels to the lungs, causing a pulmonary embolism.
Can DVT be cured?
DVT can be effectively treated, but it is not always considered cured. Treatment reduces symptoms and prevents complications.
How long does it typically take for DVT to heal?
The healing time for Deep Vein Thrombosis (DVT) can vary, but most cases improve within a few weeks to months with appropriate treatment.
What are signs that my DVT is improving?
Signs of improvement include decreased swelling, reduced pain or tenderness in the affected limb, and improved mobility over time.
Should I expect any long-term effects after my DVT heals?
Some individuals may experience long-term effects such as leg heaviness or chronic pain; follow-up care is important to monitor these symptoms.